If you have been diagnosed with diverticulitis, you may wonder what foods you should avoid.
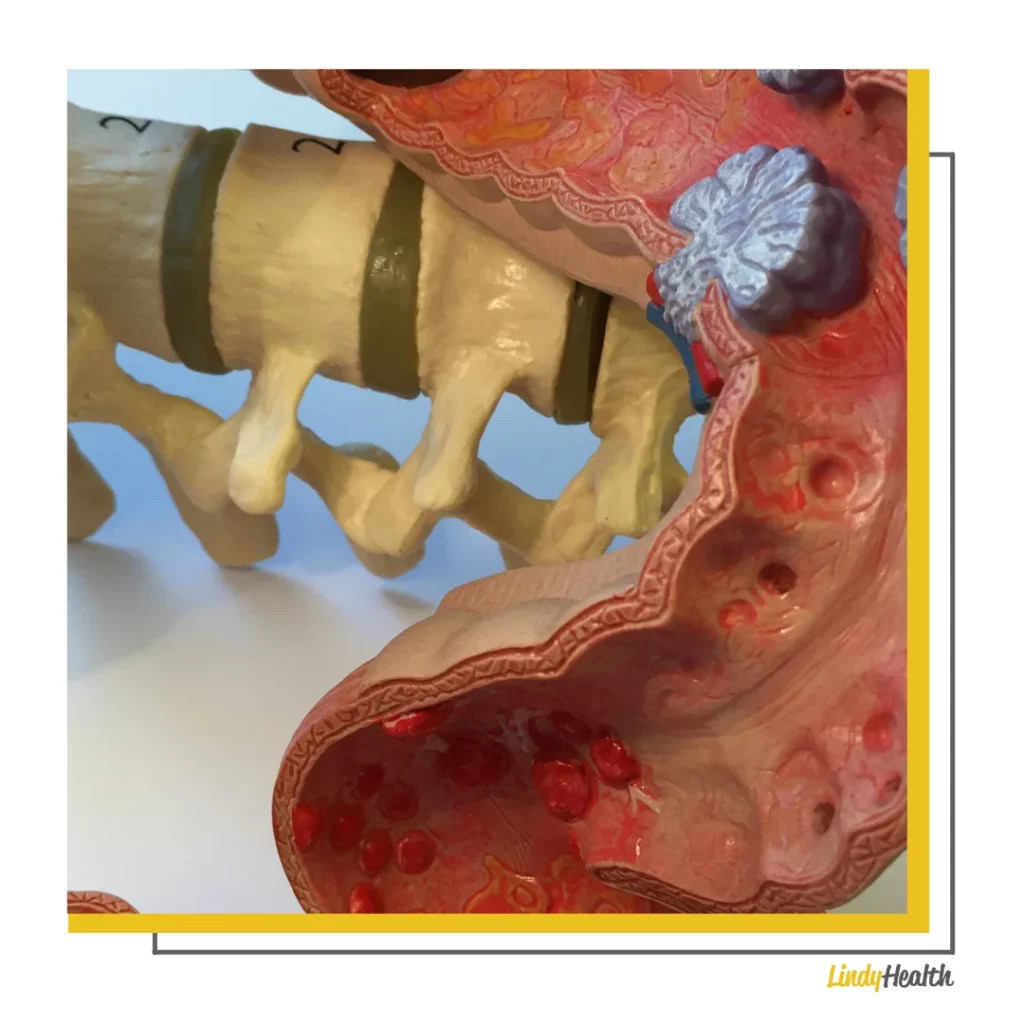
Diverticulitis is a medical condition that is caused by an infection or inflammation of the “diverticula.”
Diverticula are small little pockets the size of a coin or marble that can develop within the lining of the intestine.

This condition can develop when spots in the intestinal wall are impacted by pressure and this results in ‘bulging.’
Certain foods, health markers like obesity, and the overall health of the digestive system are all known to contribute to the development of diverticula and the progression of diverticula to diverticulitis.
Can What you Eat Impact Diverticulitis?
While some sources claim there aren’t any particular foods you need to avoid when it comes to preventing diverticulitis or making the condition worse, we know that the health of the digestive system plays a huge role in the progression of inflammation.
Previously, we were told that people with diverticula needed to avoid nuts, seeds, and popcorn.
Why? As they could “lodge” in the diverticula and cause an infection or further progression to diverticulitis. We now know this isn’t true, and that people who regularly eat these foods are actually less likely to get diverticulitis.
Those with diverticula, or diverticulitis, or simply want to avoid the problem all together: stick to a healthy diet that is high in fiber and whole foods. Avoid processed foods, refined sugars, and high FODMAP foods.

You want to avoid additional pressure within your digestive system and want food to pass quickly and effectively through the colon.
We’ll tell you exactly what foods to avoid with diverticulitis, as well as provide you with some much safer alternatives.
Refined Grains – Avoid Them
Fiber helps provide better “laxation and stool bulk,” along with supporting a healthy digestive system. This can help outnumber pathogenic bacteria with positive, probiotic bacteria in cases of uncomplicated diverticulitis.
As we have noted in our previous post, gut bacteria play a fundamental role both in the development and pathogenesis of diverticulitis.
Higher fiber intake from whole foods can also help a reduced risk/rate of increase in hunger and BMI, with higher levels of abdominal fat. Obesity and overeating are two fairly large risk factors for diverticulitis.
This also ties back into long-standing recommendations of avoiding refined grains like white bread – we probably all know by now these are not healthy foods.
Not only are they nutritionally void (any mineral content is added back in artificially), but they also provide no fiber for the digestive system and actually promote pathogenic bacteria the same way refined sugar does when eaten in abundance.
While some studies dispute any changes in the digestive effects of eating whole grains compared to refined grains, we can clearly see that there is a significant difference.
In multiple studies, consuming whole grains like barley, brown rice, or corn led to an increase in beneficial gut bacteria like Bifidobacterium, and a decrease in pathogenic bacteria like Bacteroidetes.
Mice fed whole grain oat flour has lower insulin levels, lower levels of HDL “bad” cholesterol, and high concentrations of beneficial bacteria like Lactobacillus compared to rice fed using refined flour.
Bacteroidetes like Bacteroides are gram-negative bacteria that can colonize the digestive tract and are well-known as clinical pathogens found in bacterial infections.
You don’t want these in your gut. We also know from our previous post on probiotics for diverticulitis that pathogens in the gut can promote a cycle of inflammation that leads to worsened diverticulitis outcomes.
High “FODMAP” Foods – Avoid Them
What does FODMAP mean?
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols.
These are particular fermentable carbohydrates that can lead to symptoms of digestive distress in many people, such as: gas, bloating, irritation, diarrhea and abdominal pain.
This is because these carbohydrates are resistant to digestion – when your gut bacteria try to utilize them for fuel, you get reactions in sensitive individuals.
The vast majority of them will pass through your digestive system unchanged. In the colon, they get fermented. Instead of producing methane like “good” bacteria, though, they produce hydrogen instead.

FODMAPs can also cause distention of the gut and draw water into your intestines, both of which can be triggers for diverticulitis.
FODMAPs include:
- Fructose – Sugar commonly found in many fruits and veggies, which also comprises the structure of refined sugar and added sugar.
- Lactose – The carbohydrate most commonly found in dairy products, like milk. You can often find “lactose free” substitutions.
- Galactans – Found in legumes in large amounts. This is why people often associate beans with gas!
- Fructans – Found in whole grains like rye, barley, spelt, and farro.
- Polyols – These include sugar alcohols and are important to note for those that are sugar-free but still consume “sugar free” substitutes. These are subs like xylitol, mannitol, sorbitol, maltitol, and erythritol.
In “Dietary Patterns, Foods and Fiber in IBS and Diverticular Disease,” Mark Dreher purports that a lower intake of FODMAPS (when combined with a diet high in fiber) can help reduce the risk of IBS or uncomplicated diverticulitis.
Considering FODMAPs are pretty commonly found in whole foods and plenty of healthy foods like wheat and beans, you might be wondering how to keep a high intake of fiber while avoiding FODMAPs.
There is plenty of research to substantiate the benefits of FODMAP diets for those with IBS and diverticulitis, and this means avoiding all short-chain carbohydrates in the diet.

The below are suitable substitutions that are still nutritious, healthy, and high in fiber – but do not contain FODMAPs. We also list those which contain high amounts of FODMAPs so you know what to avoid.
What to Eat with Diverticulitis:
- Bananas, blueberries (wild), raspberries, blackberries, strawberries, melons (honeydew or cantaloupe), kiwi, oranges, mandarins, and passionfruit.
- Maple syrup (sweetener substitute).
- Lactose-free milk, hard cheeses like brie, lactose-free yogurt, grass-fed butter. Milk substitutes like rice milk or oat milk.
- Carrots, potatoes, sweet potatoes, pumpkin, bok choy, butternut squash, tomatoes, leafy greens like spinach or arugula.
- Gluten-free grains like oats, buckwheat, quinoa, brown rice, or millet. Spelt bread.
- Eggs, grass-fed red meat (avoid pork), seafood.
What to Avoid with Diverticulitis:
- Apples, pears, mangos, apricots, prunes, peaches, plums.
- Fructose, high fructose corn syrups, dried fruit, fruit juice.
- Cow milk, sheep milk, goat milk (including low fat and full fat), yogurt, ice cream, cottage cheese, soft cheese like ricotta.
- Artichokes, asparagus, beetroot, brussels sprouts, broccoli, cabbage, fennel, leeks, garlic, onions, okra, shallots.
- Chickpeas, lentils, red kidney beans, black beans.
- Sugar substitutes – xylitol, mannitol, maltitol, sorbitol.
- Whole grain wheat, rye and barley.
LindyHealth has also got a comprehensive Low FODMAP vegetable guide, for those looking to incorporate more nutritious veggies into meal plans without worry over aggravating diverticulitis.
The Bottom Line – Dietary Considerations to Keep in Mind with Diverticulitis
Previously, doctors also recommended a “liquid diet” which we would advise against unless you have a severe infection – in that case, we would always suggest consulting with a medical professional immediately.
In these instances, it may be better to slowly build a higher fiber diet from starting with things like bone broth, squash soups, lactose-free yogurt, and banana peanut butter smoothies.
People typically will develop these diverticula over periods of years from continual pressure preventing food from moving through the GI tract effectively.
To combat this, and prevent the occurrence, and flare-ups – you need to ensure you consume at least 25-35 grams of fiber from whole food per day.
There are other factors to keep in mind when looking to prevent the progression of diverticulitis, and these includes:
- Moderate levels of exercise.
- Limit intake of processed & refined fats (seed oils or fried food). Those with severe cases may want to be more restrictive on saturated fat intake.
- Limit intake of red meats (only eat grass-fed beef; no pork – opt for eggs, poultry, or seafood instead).
- No NSAIDs (Aspirin or Ibuprofen) – these can damage and irritate the lining of the digestive system and promote chronic inflammation.
- Drink plenty of water, around 64 ounces daily.
- Avoid fermented foods like sauerkraut & kimchi (can eventually be reintroduced if no irritation or flare-ups). These may cause irritation in more sensitive individuals.
Ultimately, each person is different – some high-fiber foods may cause irritation on flare-ups among sensitive individuals or those with a worse case of diverticulitis.
When increasing fiber intake and eating a whole food diet, it is important to ensure you’re getting an adequate amount of water to support the increase in ruffiage for the gut.
You’ll need to ensure you communicate properly with your doctor or health care professional regarding any sort of dietary changes. Diverticulitis can be a chronic condition, despite it laying dormant – it can also unexpectedly flare.
Eating right for those with diverticulitis doesn’t have to be complicated or restrictive. Finding healthy alternatives is easy, and you will always want to center your diet on nutritious, whole food.
Let us know if you’ve had any success following a low FODMAP diet, or if certain foods have been useful for healing from diverticulitis!
- Peter MD Review 2024 – Is it a Good TRT Option? - February 27, 2024
- 5 Best SARM Companies - February 1, 2023
- Movement, Exercise, and How to Make it Stick - January 11, 2023








